Eng
Why should society deprive itself of the experiences and enthusiasm of the elderly for a short, long or indefinite period, simply because they broke their femur slipping and falling while swinging a table? Why do young working people have to spend so much of their time looking after people who need a lot of attention? This site sets the scene and offers the views and solutions proposed by Prevent SRL.
Index
- Introduction (reading time < 30 s)
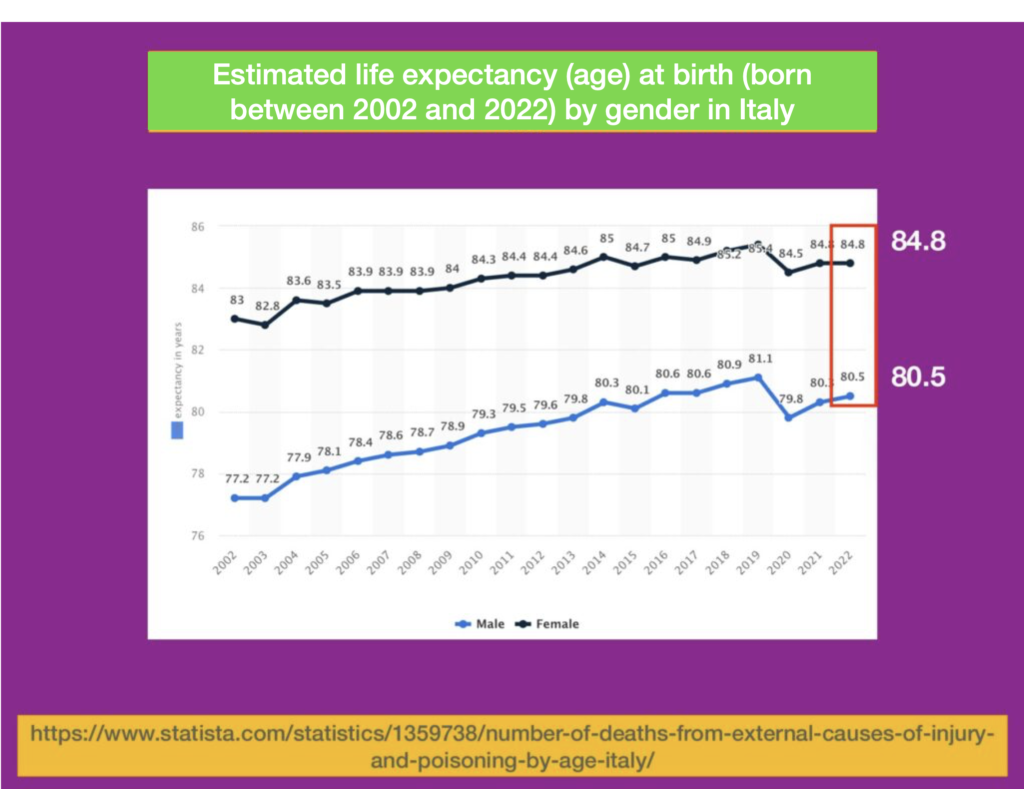
- Estimated life expectancy at birth in Italy (graph) (reading time < 30 s)
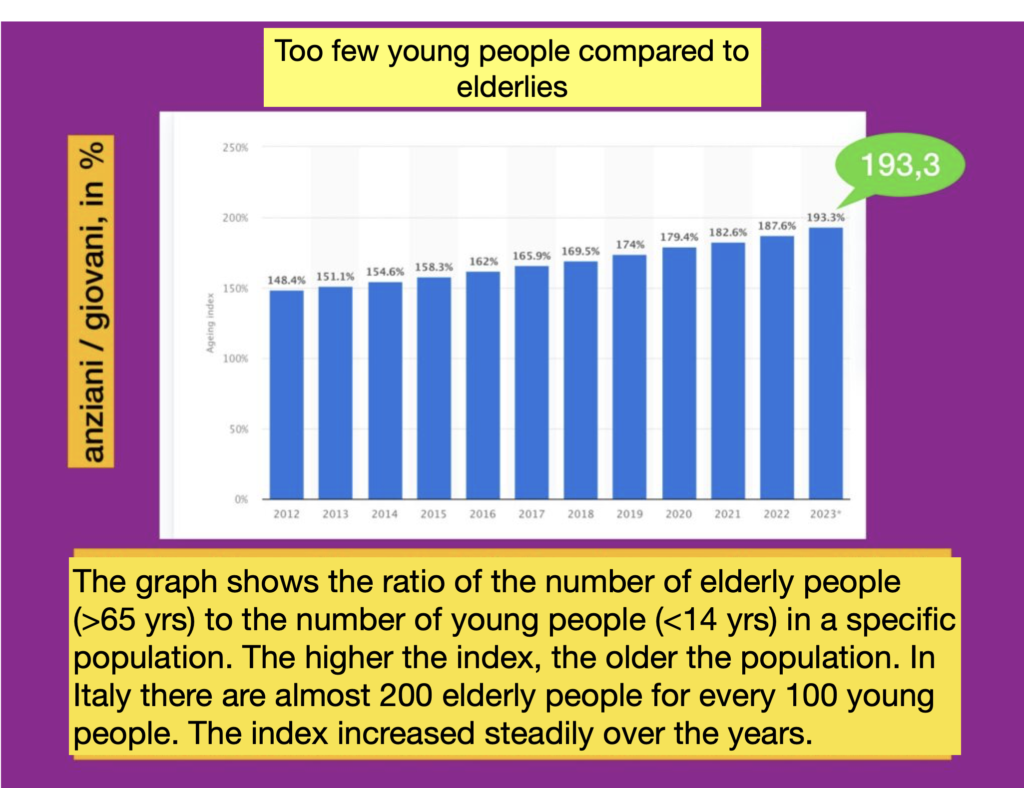
- Ageing index in Italy (chart) (reading time < 30 s)
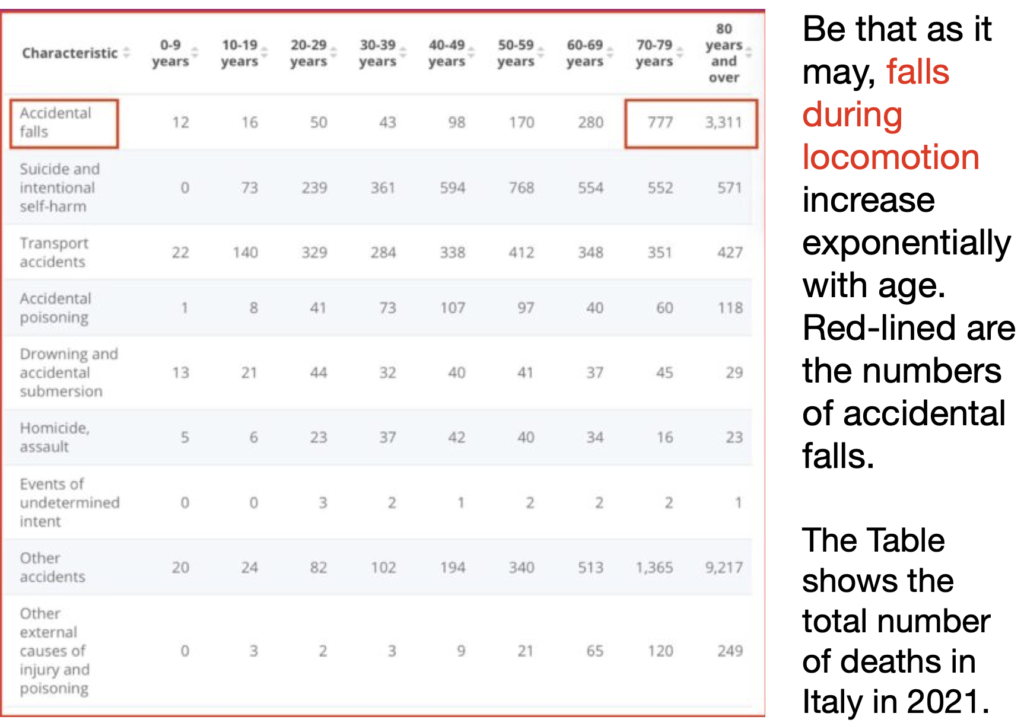
- Number of deaths due to accidental falls (chart) (reading time < 30 s)
- Prevention and rehabilitation (reading time < 30 s)
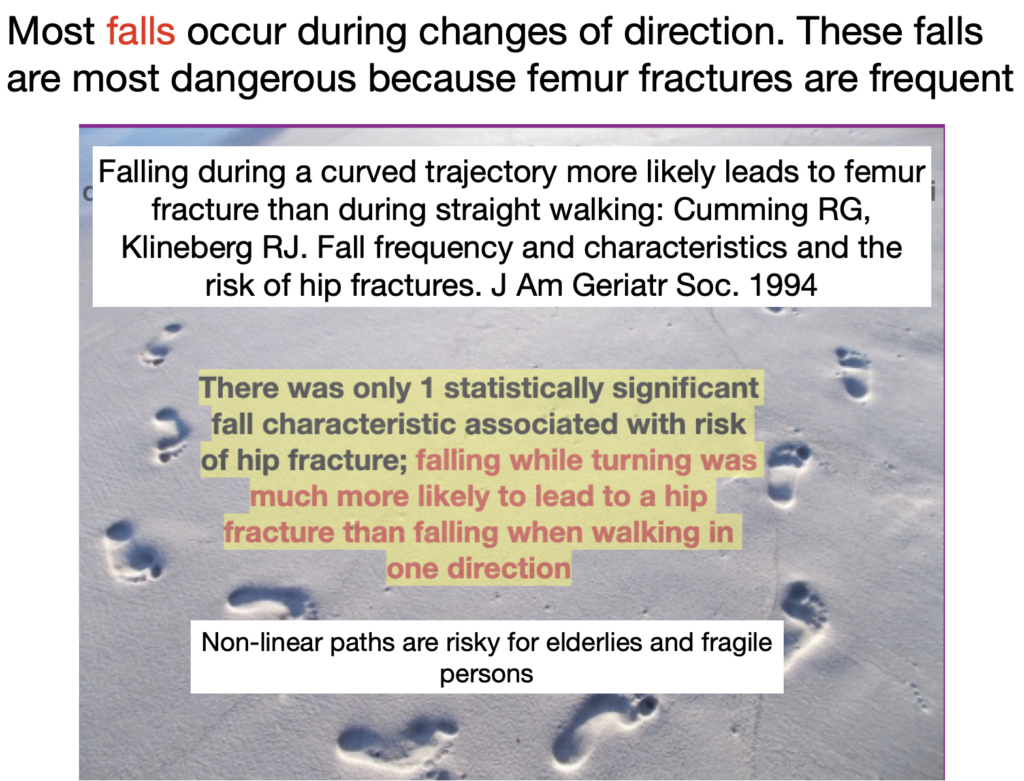
- Falls during changes in walking direction (reading time < 30 s)
- The terms of the problem (prevent and rehabilitate) (reading time < 30 min)
- Links to the Google Scholar and ORCID page of the founder of Prevent srl

.
Introduction
One can either destroy a person with a sword or deprive them of their autonomy. The first case constitutes an illegal action, the second seems to be tolerated by oblivious public health officials and policy makers.
To get an idea of the issue, one only has to spend some time in community homes for the elderly, where even those who are self-sufficient soon cease to be so and become a burden on themselves, their families and staff.
Laying aside all didactic pretensions, it is useful to do the maths. Does it cost the community more to have a self-sufficient elderly person or an elderly person who does not move or is blocked by the fear of falling or actually falls more or less ruinously? Does it cost more a preventive treatment to prevent falls or a long and difficult convalescence after the accident? Does it cost more to have a general physical rehabilitation treatment after femur osteosynthesis or a specific treatment that promotes the resumption of activity of the muscles that rotate the femur and leg in a functional context?
This site presents the state of affairs and offers the point of view and solutions proposed by Prevent srl.
.
Since newborns will have long lives, it will be important to add life to the years.
Younger people will take care of the elderly: let us work for these to be self-sufficient. The general objective is to contribute to increase disabled people’s autonomy, offering them the possibility to organize their own mobility.
Falls during locomotion increase exponentially with age
It seems so obvious that falls should be prevented and rehabilitated
In order to improve the autonomy of patients who are frail (Allison et al., 2021) due to age or impairment of sensibility and strength, or due to health conditions or multi-medication, and to restore self-sufficiency as soon as possible after a fall, it is necessary to
PREVENT: identify conditions and states that can lead to falls.
REHABILITATE: identify procedures that specifically address the functions to be strengthened, capable of rapidly improving or completely restoring locomotion, and capable of reducing the risk of falling.
People fall more easily when following curved trajectories, which require accurate anticipation of the turn, continuous fine control and effective coordination of the activity of the muscles rotating the lower limbs in relation to the pelvis.
THE TERMS OF THE PROBLEM AND THE PROPOSED SOLUTION: IMPORTANT DETAILS.
- Walking along non-straight trajectories
- The execution of curved trajectories is not trivial
- Even young disabled people have problems changing direction
- The public health problem
- The physiology of turning
- Prevention and rehabilitation
- Fitness, training, rehabilitation in sport
- The proposed device
- Training characteristics
- Limitations and differences compared to treadmill walking
- Outcome tests
- Bibliography (to search for a bibliographic entry cited in the text: double-click on the author’s name ▶ CTRL F ▶ search — to retrieve the article or its summary from the bibliography ▶ click on the author’s name
Locomotion along non-straight trajectories
- Changing direction while walking is a typical activity in daily life, necessary to perform basic functional activities such as turning around a table or walking a curved path along a footpath. A successful turn requires effective coordination between the movements of the lower limbs and those of the trunk and pelvis.
- When walking along a curved trajectory, particularly with limited radii of curvature, asymmetric changes in the stride length of the two limbs occur (the stride of the leg towards the inside of the curve is shorter as a function of the angle of curvature, while the stride of the outer leg has a comparable length to when walking linearly at the same speed) and the ground reaction forces that control the locomotion direction are appropriate to orient the body in the new direction (Courtine and Schieppati, 2003; Turcato et al. , 2015).
- Minimal but essential changes in postural reactions (such as mid-lateral trunk tilt) are also required to adjust walking speed when the turn is initiated (Turcato et al., 2015). These synergies lead to a critical body position tilted inwards in order to prevent the body from being ‘thrown’ outwards from the desired path by the centrifugal force caused by the execution of the curved trajectory.
- Two important functions are therefore called upon: the control of posture and balance on the one hand (Brinkerhoff et al., 2023) and the control of the asymmetry of the steps of both legs on the other. The segment represented by the trunk and pelvis is the one that allows the execution of effective changes of direction while walking. Furthermore, rotation (intra- and extra-rotation of the legs) is possible thanks to the coxo-femoral joint on which numerous muscles insist (Figure 1 below).
Execution of curved trajectories is not trivial
- It is well known that changing direction during walking is difficult in patients with Parkinson’s disease, who often stop or start taking small steps before changing direction (Guglielmetti et al., 2009; Turcato et al., 2018; Godi et al., 2019) or rotate slowly ‘en-bloc’ (Mellone et al., 2016). In Parkinson’s disease, prolonged exercise leads to greater mobility and allows the learning of strategies to control the body’s rotational movement and the necessary postural adjustments (Godi et al., 2017), including those affecting the trunk (Carpenter et al., 1999), controls that are progressively lost as the disease progresses. Turning slowly results in similar alterations in eye movements, rotation kinematics and gait characteristics in the group with PD and in healthy controls (Mancini et al., 2015). Training using different turning directions and speeds can improve coordination, as well as increase confidence and reduce the risk of falling (Khobkhun et al., 2022).
- Multiple sclerosis causes disruption of neurological networks in the central nervous system, commonly impairing functions such as mobility, muscle strength and coordination. The prevalence of falls is about 56 per cent in people with MS and about 37 per cent of people who fall are classified as frequent fallers (Arpan et al., 2022). There is evidence that frailty in multiple sclerosis is modifiable (Zanotto et al., 2024). Stroke patients present walking disorders due to damage to motor and sensory pathways. Patients with hemiparesis due to a cerebral vascular accident also have incorrect postures and problems in walking in curved trajectories (Godi et al., 2010; Chisholm et al., 2015; Jin et al., 2023), as well as having obvious problems in foot positioning during even linear walking due to the general unstable gait pattern. These patients present asymmetry of the lower limbs due to the lack of control of muscle activation and cannot easily support their weight on the paretic leg inside the curvature. Disturbances in the synchronism of coordination between the lower limbs are indicators of stability control during walking (Singer et al., 2013).
Even young disabled people have problems changing direction
- The strategy of changing direction during walking is also impaired in children with infantile cerebral palsy (Dixon et al., 2014; Brégou-Bourgeois et al., 2014). Recently, differences in energy expenditure of walking with turns compared to a linear walk have been measured in children (Crossley et al., 2018). There are indications that (linear) walking in cerebral palsy patients can be partly improved if intensive coordination dynamics therapy is administered for 1 to 2 years (Schalow and Jaigma, 2005) including by means of exoskeletons (Patanè et al. 2017), but no effects on direction changes are known. For more details, see (Cappellini et al., 2020). Incorrect relationships of the bone anatomy cause a decrease in muscle power, because the corresponding muscles do not work in the plane for which they were designed. This makes the muscle less efficient and causes the patient to spend more energy walking (Novacheck and Gage, 2007; Böhm and Döderlein, 2012) and complicates coordination between motor synergies. Similarly, stepping exercises (stepping on and off a step) have been recommended for children with motor coordination disorders (Inacio et al., 2023), but these exercises appear to be very poor at promoting coordination of more common and more complex movements. Instead, exercises focused on the trunk seem to have a better effect (Pierret et al., 2023; van Dellen et al., 2023). Children with cerebral palsy exhibit greater postural instability than their peers with typical development (Szopa and Domagalska-Szopa, 2024). It has recently been shown that dynamic postural stability does not fully mature until the age of 10 years or more (Mani et al., 2021), suggesting that an intervention such as the one described below (walking in place on the rotating platform, see Figure 2) can also validly operate in children with cerebral palsy.
The public health problem
- Steps occurring during turning represent approximately 35-40% of all steps in a typical day for a normal adult subject; the daily number of steps in turning increases when in confined spaces such as in a flat. Aging people change direction less efficiently, as evidenced by the degradation of kinematics and neuro-muscular modulation (Baird and Van Emmerik, 2009; Robinovitch et al., 2013; Asmidawati et al., 2014). In the elderly, systematic reviews of the literature have established that exercise reduces falls, but the most effective types of exercise are unknown (Lord and Close, 2018; Sibley et al., 2021). The frequency of falls increases in the elderly with lower limb rotation deficits. Sedentary lifestyle, which is unfortunately extremely common in the elderly and even more so in the frail (who may have multiple diseases, multiple treatments with different medications at the same time, and prolonged bed rest) produces sarcopenia (Cruz-Jentoft & Sayer, 2019). Falls during rotation are responsible for eight times more hip fractures than during walking along a straight trajectory (Cumming and Klineberg, 1994; Thigpen et al., 2000; Almajid et al., 2020). It has been suggested that measures of turn-based gait production efficacy predict (and may prevent) recurrent falls in community-dwelling elderly (Leach et al., 2018). It is worth mentioning the enormous social and economic cost of fall-related fractures (Ambrose et al., 2013; Veronese and Maggi, 2018). There is a recent paper on ‘Frailty in Italy’ (Vetrano, 2022) and another equally recent one by the World Health Organisation that discusses the need for rehabilitation in Europe and highlights the problems associated with these needs (Health Workforce and Service Delivery, 2022).
Physiology of curved walking
- The muscles responsible for the rotation of the lower limb along the longitudinal axis are the pelvic muscles, which rotate the femur in its coxo-femoral joint (Figure 1, A and B). These muscles are numerous and require special coordination (Ventura et al., 2015). The pelvis in turn pivots on the supporting leg and the trunk pivots on the pelvis, causing the body, including the neck and head, to be properly oriented to the walking trajectory to be executed.
- Coordination between the neural commands directed to the pelvic muscles (which are asymmetrically active during the walk between the right and left leg) and to the muscles of the spine is critical for the correct execution of the curved trajectory.
- The weight of the body, whose centre of mass is approximately on the vertical of the trajectory of the inside foot (or even towards the centre of the curve, outside the distance between the foot supports) requires that the pelvis and spine muscles are able to produce adequate forces to maintain dynamic balance during the execution of the path along a curved trajectory.
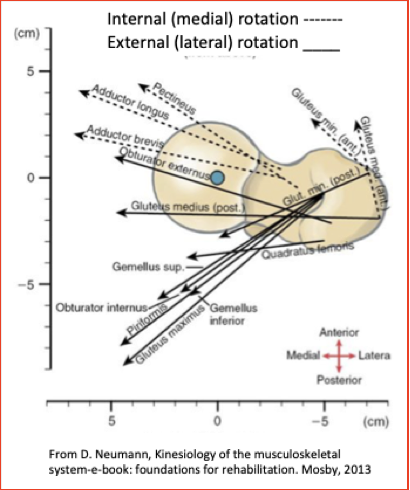
Figure 1. Direction of the muscle forces that produce intra- and extra rotation of the lower limb.
Prevention and Rehabilitation
- It therefore seems appropriate to design a physical treatment capable of exercising the intra- and extra-rotator muscles of the leg on the pelvis in a manner consistent with their function during curved walking.
- This activity is aimed at stimulating neuro-muscular coordination and at the same time strength development in the aforementioned muscles. Indeed, it is known that sensory information about the ongoing movement from intramuscular receptors provides an important input for learning and reinforcing the execution of a certain movement (Ziemann et al., 2001; Rosenkranz and Rothwell, 2012). The ability to ‘learn’ appropriate co-ordination through the use of the rotating platform is evidenced by the persistence of turning on oneself while walking in place with eyes closed (i.e. without visual spatial reference) after the rotating platform has stopped (Sozzi and Schieppati, 2016).
- It is necessary to address the issue of strengthening and coordination of the muscles responsible for intra- and extra-rotation of the lower limbs, both for a) preventive purposes i.e. to reduce the likelihood of falls due to insufficient strength development in sedentary elderly and frail subjects (Álvarez-Millán et al, 2023), for b) rehabilitative purposes (rehabilitation of impaired or slow gait for problems related to neurodegenerative diseases) or c) therapeutic purposes (restoration of locomotor function along non-linear paths after hip or pelvic fractures (Fox et al., 1998; Damm et al., 2018). Incidentally, muscle and coordination strengthening is also appropriate prior to hip replacement surgery (Fairhall et al., 2022).
- Despite the wealth of known physiotherapeutic exercises and the use of the corresponding equipment, which are offered in a hospital or community setting or at home (independently or guided), there is no simple instrument on the market that a) can stress activities normally neglected during conventional rehabilitation treatment, b) can be used by the healthy or elderly or frail individual with the ease and safety with which he or she uses an exercise bike or a simple treadmill.
- Until now, a frequently used device has been the normal linear treadmill. An evolution of the normal treadmill is the so-called ‘split-belt’ treadmill, in which the bands move at different speeds, producing an asymmetrical path – but always in a straight line. For example, in Parkinson’s disease, the ‘split-belt’ treadmill has been used but did not produce appreciable results in post-treatment walking (Hulzinga et al., 2023).
- There are also complex, wearable, motorised exoskeletons, which are innovative devices that can aid activities of daily living – but the production of curved gait is not envisaged (Wright et al., 2023). Furthermore, they are not widely adopted in clinical settings due to the ‘disconnect’ between the needs of exoskeleton users and the needs of the engineers designing the devices (Morris et al., 2023), as well as entailing a number of risks that are not always evaluated (Massardi et al., 2023). They may be considered as aids rather than re-enabling devices, but they still do not address the problem of coordinating movements to promote or produce gait rotation when turning (Ivanenko et al., 2023), a problem that is instead specifically addressed by the device proposed here. Several exoskeletons fix the pelvis and limit mediolateral movements. However, mediolateral displacements of the centre of mass towards the supporting leg are a crucial component of normal gait. In physiological gait, this is achieved with a sinusoidal trajectory of the pelvis, while the thorax is kept relatively stable above it.
- In none of the above cases is it possible to intervene on the intra- and extra-rotation of the legs, let alone the complex control of posture and balance that necessarily accompanies the production of turns or walking on curved trajectories. Walking on the spot rotating on oneself along the vertical axis of the body represents a specific condition that favours dynamic control of posture and coordination between the legs and trunk. Furthermore, it represents a way to foster coordination between pelvis and trunk in the most natural way possible (van Dellen et al., 2023). The rotating platform on which one walks in place with the centre of mass placed approximately along the vertical of the body and the feet marching around the centre of curvature allows intra- and extra-rotation of the legs avoiding any head rotation and vestibular stimulation that causes disorientation, dizziness, imbalance and falls.
Fitness, training, sport rehabilitation
- In sports, it is relevant to consider that the exercise imposed by the rotating platform can last for an indefinite period of time decided by the coach or the athlete himself, leading to optimal development of the muscles involved and optimal coordination of the pelvic musculature with the trunk and lower limb musculature. An instrument capable of imposing rotations at different speeds while walking on the spot appears essential for training Repeated Sprint Ability in football, for example. Examples of other sports activities that involve rotational movements on oneself are basketball, discus and hammer throwing, skiing, dancing, golf, and tennis (Wang et al., 2022).
- The rehabilitation of various sports-related injuries can be addressed with the specific exercises permitted by the use of the rotating platform. One example is the complicated and prolonged rehabilitation of knee ligament injuries, which makes it possible to transmit rotation of the femur to the leg. This rehabilitation to date follows less than complete protocols (Rodriguez et al., 2020; Kasmi et al., 2021; Lin, 2023).
The proposed device
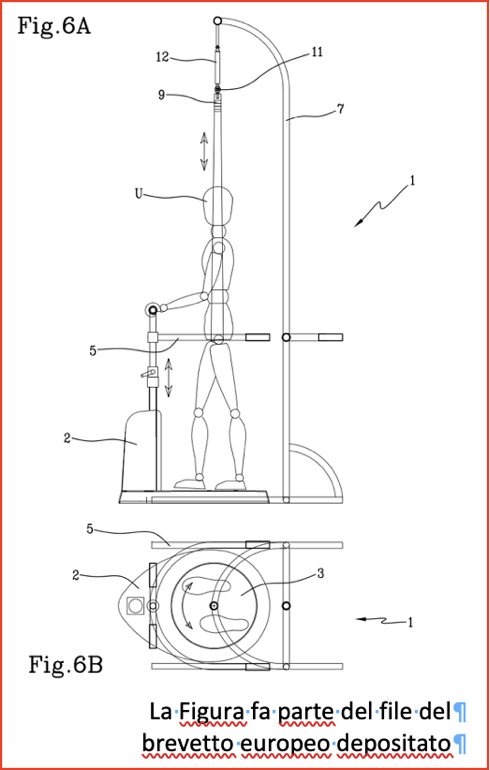
Figure 2. Overall scheme of the device (Pat Pend) TM. The European patent application was filed on 26 Apr 2023 under No. 23169980.2 for: DEVICE FOR PHYSIOTHERAPY TREATMENTS).
- It is therefore appropriate to provide a device capable of stimulating the rotation of the legs on the trunk. The device consists of a rotating horizontal disc on which the subject ‘walks/steps in place’ with head and trunk stabilised in space by the grip of a fixed handrail. This device is able to train the rotational movements of the lower limbs that normally occur when walking in curved trajectories and allow the learning (or re-learning) of the underlying neuromuscular coordination (Figure 2). A European patent application was filed on 26 Apr 2023 under No. 23169980.2 for: DEVICE FOR PHYSIOTHERAPY TREATMENTS).
- Briefly, the action of the device can be described as follows. When the right foot rests on the rotating disc in a clockwise direction, the right foot and leg are passively extra-rotated (the rotation of the tibia on the foot and that of the femur on the knee are of minimum amplitude while that at hip level is maximum). During the next phase of lifting the rotated limb (as the subject continues to march in place), while the other limb is on the ground (resting on the platform), the subject actively and naturally brings the lower limb back to a ‘straight’ position and then places it back on the rotating disc and so on. A similar sequence occurs for the left limb, which will instead be intra-rotated by the rotating disc. A sequence of intra- and extra-rotation will then occur for clockwise rotations. The same sequence of leg rotations will occur in the opposite direction when the turntable rotates anti-clockwise. Other movements are provided, such as short, rapid impulsive rotations of the platform (see below). Although the use of postural perturbations has shown positive results in various areas of posture and gait rehabilitation (Ribeiro de Souza et al., 2023), there is to date no dedicated system for rotator muscle perturbations.
- It is sufficient for the rotating disc to have a diameter of 50 cm in order to easily perform its function. The subject will be leaning with the upper limbs against a support that allows the primary position (looking forward without head-neck rotation) of the upper torso and head to be maintained. The primary position of the upper body, with the head virtually fixed in space, avoids any vestibular rotatory stimulation that could cause dizzy episodes and falls (as when the subject rotates on itself for a few seconds on fixed ground). The subject walks in place with its vertical axis passing through the centre of mass of the body, which is projected onto a point on the platform that forms the pivot of the rotation.
- For clinical use in critically ill patients, a lightweight sling is provided (Figure 2). It is attached to support the subject vertically, and the platform does not move unless the ‘seat belt’ is fastened (as in cars). This function is optional if the training is supervised. It is just worth mentioning that since the subject is leaning and with his feet around the centre of the platform, the vertical of the body corresponds to the centre of rotation. Therefore, since its centre of mass is not stressed by transverse perturbations, the risk of falling is negligible. The necessary safety precautions are provided. Supporting the handrail will be compulsory, on pain of stopping the platform. Any failure of the legs will also cause the rotation to stop. A lock button will be available.
- The angular speed of the rotating disc can vary in order to adapt the speed of rotation of the body while walking on the platform to the subject’s abilities (from slow to progressively faster speed both during one treatment and in repeated treatment sessions). The speed and duration of rotation can be pre-set by the subject at home, or in the clinical setting by the physiotherapist. The rotation period may last several minutes. The rotation may have constant or variable angular velocity. It can be continuous clockwise or continuous counterclockwise or have periods with increasing and decreasing angular velocities and with reversal of the direction of rotation. Several rotation patterns are pre-set and retrievable by the subject (or physiotherapist) through interaction with an accessible tablet. Other patterns can be easily implemented off-line and then incorporated into the pre-set options. Other movements of the rotating platform are envisaged, such as a. rotations whose direction gradually changes during the treatment session, in order to distribute muscular stresses with equal importance to both the right and left during the treatment session, b. short, rapid impulsive rotations of the platform (see below). In fact, although the use of postural perturbations during standing and walking has yielded some positive results in various areas of posture and gait rehabilitation (Ribeiro de Souza et al., 2023), there is to date no dedicated system for rotator muscle perturbations. Other patterns can be easily implemented. The duration of the platform rotation can also be very prolonged, configuring a ‘gait endurance’ type of training (Petrini, 2023).
- The rotating ‘system’ (rotating platform and marching subject) is equipped with a simple accelerometer that records the cadence of the footstrike and a heart rate monitor.
- A tablet collects platform rotation data and foot strike cadence and creates an excel table of these variables, which can be accessed and downloaded to a PC for later off-line analysis. An acoustic and/or visual metronome can be set from the tablet, so that the ‘imposed’ rhythm can be compared with the actual rhythm.
- At this early stage of the device’s development, there are no plans to implement other functions, such as the vibration of the trunk muscles, which has been shown to be capable by itself of causing deviations in the locomotion trajectory (Bove et al., 2001; Courtine et al., 2007) and inducing body rotations during walking in place (Sozzi et al., 2019).
- The use of the platform is easy and safe: the person simply walks/steps in place (with or without a sling, depending on the condition), at the pace they prefer (or at the pace set by the metronome) while holding onto a handrail. The angular speed of the platform is set through the use of buttons on the tablet (which limits the choices to non-threatening rotations).
- End-user acceptance of the adoption and use of a prototype of the new system was evaluated and proved to be positive. Although some minimal effort may be required to use the system during prolonged treatment, the effort is perceived as worthwhile as users expect that the device will improve their walking performance and influence their social life.
- It is sufficient for the rotating platform to have a diameter of 50 cm in order to easily fulfil its function. The device is movable and transportable because it has a modest weight (≈ 20 kg) and can be disassembled into a few pieces with negligible bulk. When assembled, it occupies an area of no more than one square metre, allowing it to be placed even in small rooms or to locate several in the same room. It is safe, both mechanically and electrically. The cost for the healthcare facility or private individual who will be equipped with it will be low (depending on the characteristics of mass production).
The characteristics of the training (see an animation at the end of this page, Figure 4)
- This type of exercise relieves the central nervous system from the ‘effort’ to maintain balance, critical activity during the nomal walk in patients with problems of locomotion of different nature, thanks to the fact that the upper body of the subjects (the head, the shoulder girdle and the trunk) is practically stationary (or rather little mobile) because they hold with their hands to a support while marching on the place.
- This allows subjects to perform with ‘tranquility and coolness’ and for a long time the movements imposed by the platform. The rotation along the major axis of the lower limb during the stepping in place is both passive, during the support of the foot, and active during the lifting; in both cases does not involve any unusual or ‘strange’ movement or the deliberate learning of a new or unusual motor sequence. The acoustic cueing given by the metronome, and a long-lasting task help patients with PD to maintain a constant stepping rate despite the ‘virtual’ curvature of the path trajectory, helping them to overcome conditions that normally lead to destabilization, rhythm alterations and freezing (Spildooren et al., 2010; Rutz and Benninger, 2020).
- As for the mentioned rapid rotations of small amplitude, it is known that exercises based on postural perturbations are able to prevent falls in the elderly. Perturbation-based balance training (PBT) can have several characteristics (Brüll et al., 2023). The movements of this platform propose an activity that summarizes the salient aspects of PBT and at the same time causes stress on the posture and muscles that generate the rotations of the lower limbs. The advantages of this procedure have so far only been described in the linear path (Castano, 2023).
- The many features offered by this training are in line with recent indications relating to reablement programs or restorative treatments in elderly patients admitted to the community (see the recent review article by Lewis et al., 2021). In particular, reference is made here to function-focused treatments that aim to improve degraded motor functions (for reduced coordination or sarcopenia or other common conditions related to hypo-mobility in the elderly) and thus prevent serious problems such as falls. The proposed exercise is a typical ‘proprioceptive’ exercise (Sherrington et al., 2019) suitable to prevent falls in the elderly. The articulated options of the control of the movement of the platform offer the physiotherapist the freedom to act both on the duration and speed of the rotation of the platform according to his experience during the treatment of a particular old and fragile patient or subject.
- It is worth mentioning that on-site stepping on the rotating platform does not cause high impact on the foot support base (as is the case with the ‘normal’ treadmill) because it lacks the ‘forward thrust’ imposed by the treadmill, and even less it produces excessive pressure on the joints of the leg and pelvis, thus eliminating any risk of injury from impact.
- As a caveat, stepping in place on the rotating platform simulates/stimulates the intra- and extra-rotation of the lower limbs with respect to the pelvis, but not the inclination of the body towards the center of the curvature of the trajectory to generate the centripetal force. On the other hand, marching on the spot has the advantage of minimizing the movements of the head, making negligible the vestibular stimulation and the effects of opto-kinetic stimulation. Even the center of mass of the body, which normally moves with considerable kinetic energy during linear walking, remains practically in situ. Further, the rotating support base does not necessarily require the generation of the displacement of the feet of several tens of centimeters in the sagittal plane as it happens in straight walking on linear treadmill.
- Of note, stepping on the rotating platform exerts little load on the hip, as produced by the ‘normal’ walk on linear treadmill due to the heel strike (for references see Palmowski et al., 2021). Since the body is always aligned vertically, as already mentioned, the foot support during the march on the spot configures a negligible load (Kuster 2002). In this way, the training can last even for long periods in the absence of the activation of the muscles that stop the fall of the body (Honeine et al., 2013). Note here that this type of exercise can also be performed wearing an ankle-foot orthosis (AFO) or knee, ankle, foot (KAFO) (Zancan et al., 2004), which could be regularly worn even by patients with spastic paresis (or by young people with CP) (Bayón et al., 2023).
- Importantly, various easy tests are available to assess the ability to rotate (see below). The modified Figure-of-8 test (Zancan et al., 2021) mentioned below (Figure 3) can be used together with the platform for preventive, evaluative or rehabilitative purposes when you want to solicit and assess the mechanisms of production of anticipatory and compensator adjustments during the walk along curvilinear trajectories and measure the effects of treatment.
Outcome Tests
- There is a range of (pre-post) tests suitable for assessing the treatment outcome. The ‘post’ assessment can be set after a single treatment and/or after each of the subsequent treatments and at the end of the entire planned treatment.
- The 360° rotation test is a measure of dynamic balance. The person undergoing the test rotates at least 360 degrees while the completion time and/or number of steps taken to complete the turn are recorded.
- The Freezing of Gait questionnaire. See in Giladi et al. (2000).
- The Timed-Up-and-Go (TUG) test. The results correlate with the risk of falling.
- The Figure-of-8 test. See Odonkor et al. (2013), Zancan et al. (2021), and Lowry et al. (2022). Figure 3 below (Zancan et al. 2021) shows the 20-metre path, printed on a large, thin but robust plastic sheet. The subject travels along a linear section, followed by a sharp right turn and a complete counterclockwise circle. The latter continues in another circle to walk clockwise, the route ends with another linear section.
- The L-test. See Cetin and Erel (2022).
- The use of some relevant measurement scales (e.g. the Falls Efficacy Scale-International and the modified Elderly Mobility Scale) is briefly summarised in Hasebe et al. (2022) and Saito et al. (2023).
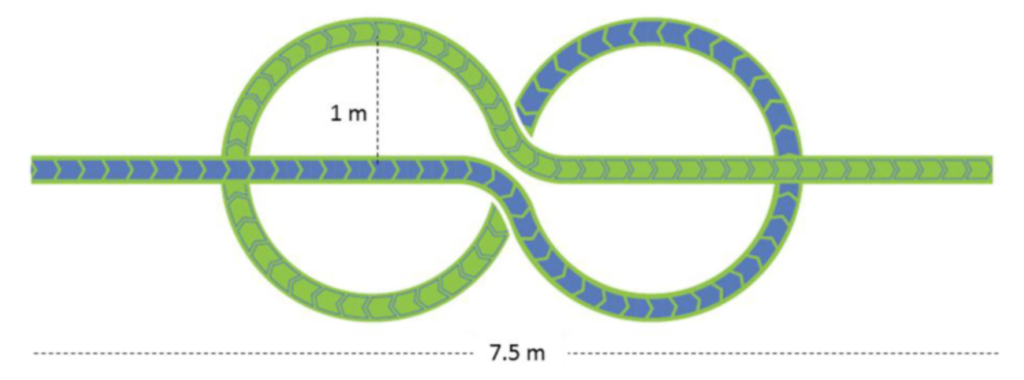
Figure 3.
Bibliography
Alcock L, Galna B, Lord S, Rochester L. Characterisation of foot clearance during gait in people with early Parkinson׳s disease: Deficits associated with a dual task. J Biomech. 2016, 49:2763-2769.
Almajid R, Goel R, Tucker C, Keshner E. Balance confidence and turning behavior as a measure of fall risk. Gait Posture. 2020 Jul;80:1-6.
Álvarez-Millán L, Castillo-Castillo D, Quispe-Siccha R, Pérez-Pacheco A, Angelova M, Rivera-Sánchez J, Fossion R. Frailty Syndrome as a Transition from Compensation to Decompensation: Application to the Biomechanical Regulation of Gait. Int J Environ Res Public Health. 2023;20:5995.
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013 May;75(1):51-61.
Arpan I, Shah VV, McNames J, Harker G, Carlson-Kuhta P, Spain R, El-Gohary M, Mancini M, Horak FB. Fall Prediction Based on Instrumented Measures of Gait and Turning in Daily Life in People with Multiple Sclerosis. Sensors (Basel). 2022 Aug 9;22(16):5940.
Asmidawati A, Hamid TA, Hussain RM, Hill KD. Home based exercise to improve turning and mobility performance among community dwelling older adults: protocol for a randomized controlled trial. BMC Geriatr. 2014 Sep 8;14:100.
Baird JL, Van Emmerik RE. Young and older adults use different strategies to perform a standing turning task. Clin Biomech (Bristol, Avon). 2009;24(10):826-32.
Bayón C, Hoorn M v, Barrientos A, Rocon E, Trost JP, van Asseldonk EHF. Perspectives on ankle-foot technology for improving gait performance of children with Cerebral Palsy in daily-life: requirements, needs and wishes. J NeuroEngineering Rehabil 2023 20, 44.
Becker C, Chiari L. What videos can tell us about falling. Lancet. 2013 Jan 5;381(9860):8-9.
Bekkers EMJ, Mirelman A, Alcock L, Rochester L, Nieuwhof F, Bloem BR, Pelosin E, Avanzino L, Cereatti A, Della Croce U, Hausdorff JM, Nieuwboer A. Do Patients With Parkinson’s Disease With Freezing of Gait Respond Differently Than Those Without to Treadmill Training Augmented by Virtual Reality? Neurorehabil Neural Repair. 2020;34:440-449.
Benn NL, Jervis-Rademeyer H, Souza WH, Pakosh M, Inness EL, Musselman KE. Balance Interventions to Improve Upright Balance Control and Balance Confidence in People With Motor-Incomplete Spinal Cord Injury or Disease: A Systematic Review and Meta-analysis. Arch Phys Med Rehabil. 2024:S0003-9993(24)01162-6.
Böhm H, Döderlein L. Gait asymmetries in children with cerebral palsy: do they deteriorate with running? Gait Posture. 2012 Feb;35(2):322-7.
Brégou-Bourgeois A, Mariani B, Aminian K, Zambelli PY, Newman CJ. Spatio-temporal gait analysis in children with cerebral palsy using foot-worn inertial sensors. Gait Posture. 2014;39(1):436-42.
Brinkerhoff, S.A., Murrah, W.M. & Roper, J.A. The relationship between gait speed and mediolateral stability depends on a person’s preferred speed. Sci Rep 2023 13, 6056.
Brown S, Martinez MJ, Parsons LM. The neural basis of human dance. Cereb Cortex. 2006 Aug;16(8):1157-67.
Brüll L, Hezel N, Arampatzis A, Schwenk M. Comparing the Effects of Two Perturbation-based Balance Training Paradigms in Fall-prone Older Adults: A Randomized Controlled Trial. Gerontology 2023, Mar 15.
Cappellini G, Sylos-Labini F, Dewolf AH, Solopova IA, Morelli D, Lacquaniti F, Ivanenko Y. Maturation of the locomotor circuitry in children with cerebral palsy. Front. Bioeng. Biotechnol. 2020 8:998.
Carpenter, M., Allum, J. & Honegger, F. Directional sensitivity of stretch reflexes and balance corrections for normal subjects in the roll and pitch planes. Exp Brain Res 1999 129, 93–113.
Castano, C. Gait Strategies While Walking with Discrete Perturbations on a Self-Paced Treadmill (2023). Electronic Theses and Dissertations, 1532.
Cetin SY, Erel S. Investigation of the validity and reliability of the L test in children with cerebral palsy. Physiother Theory Pract. 2022 Jan;38(1):182-188.
Chisholm AE, Qaiser T, Lam T. Neuromuscular control of curved walking in people with stroke: Case report. J Rehabil Res Dev. 2015;52(7):775-83.
Courtine G, Schieppati M. Human walking along a curved path. I. Body trajectory, segment orientation and the effect of vision. Eur J Neurosci. 2003 Jul;18(1):177-90.
Courtine G, De Nunzio AM, Schmid M, Beretta MV, Schieppati M. Stance- and locomotion-dependent processing of vibration-induced proprioceptive inflow from multiple muscles in humans. J Neurophysiol. 2007 Jan;97(1):772-9.
Courtine G, Song B, Roy RR, Zhong H, Herrmann JE, Ao Y, Qi J, Edgerton VR, Sofroniew MV. Recovery of supraspinal control of stepping via indirect propriospinal relay connections after spinal cord injury. Nat Med. 2008 Jan;14(1):69-74.
Crossley SGM, Mackintosh KA, Wilson RP, Lester LJ, Griffiths IW, McNarry MA. Energy expenditure associated with walking speed and angle of turn in children. Eur J Appl Physiol. 2018 Dec;118(12):2563-2576.
Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019 Jun 29;393(10191):2636-2646. doi: 10.1016/S0140-6736(19)31138-9.
Cumming RG, Klineberg RJ. Fall frequency and characteristics and the risk of hip fractures. J Am Geriatr Soc. 1994 Jul;42(7):774-8.
Damm P, Zonneveld J, Brackertz S, Streitparth F, Winkler T. Gluteal muscle damage leads to higher in vivo hip joint loads 3 months after total hip arthroplasty. PLoS ONE. 2018;13(1):e0190626.
Dixon PC, Stebbins J, Theologis T, Zavatsky AB. Ground reaction forces and lower-limb joint kinetics of turning gait in typically developing children. J Biomech. 2014 Nov 28;47(15):3726-33.
Fairhall NJ, Dyer SM, Mak JC, Diong J, Kwok WS, Sherrington C. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst Rev. 2022 Sep 7;9(9):CD001704.
Filippi, G. M., Rodio, A., Faralli, M., Ricci, G., & Pettorossi, V. E. Plastic changes induced by muscle focal vibration: a possible mechanism for long-term motor improvements. Frontiers in Neuroscience, 2023, 17, 231.
Fox KM, Hawkes WG, Hebel JR, Felsenthal G, Clark M, Zimmerman SI, Kenzora JE, Magaziner J. Mobility after hip fracture predicts health outcomes. J Am Geriatr Soc. 1998 Feb;46(2):169-73.
Giladi N, Shabtai H, Simon ES, Biran S, Tal J, Korczyn AD. Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat Disord. 2000 Jul 1;6(3):165-170.
Gill TM, Allore H, Guo Z. The deleterious effects of bed rest among community-living older persons. J Gerontol A Biol Sci Med Sci. 2004 Jul;59(7):755-61.
Godi M, Nardone A, Schieppati M. Curved walking in hemiparetic patients. J Rehabil Med. 2010 Oct;42(9):858-65.
Godi M, Giardini M, Schieppati M. Walking Along Curved Trajectories. Changes With Age and Parkinson’s Disease. Hints to Rehabilitation. Front Neurol. 2019 May 24;10:532.
Godi M, Giardini M, Nardone A, Turcato AM, Caligari M, Pisano F, Schieppati M. Curved Walking Rehabilitation with a Rotating Treadmill in Patients with Parkinson’s Disease: A Proof of Concept. Front Neurol. 2017 Feb 28;8:53.
Grasso R, Ivanenko YP, Zago M, Molinari M, Scivoletto G, Castellano V, Macellari V, Lacquaniti F. Distributed plasticity of locomotor pattern generators in spinal cord injured patients. Brain. 2004 May;127(Pt 5):1019-34.
Guglielmetti S, Nardone A, De Nunzio AM, Godi M, Schieppati M. Walking along circular trajectories in Parkinson’s disease. Mov Disord. 2009 Mar 15;24(4):598-604.
Hasebe Y, Akasaka K, Otsudo T, Hall T, Yamamoto M. Effects of incorporating elliptical trainer exercise during rehabilitation on physical function and self-reported outcomes after total hip arthroplasty: a randomized controlled trial. J Phys Ther Sci. 2022 Mar;34(3):230-235.
Health Workforce and Service Delivery. The need for rehabilitation services in the WHO European Region. 2022. https://www.who.int/europe/publications/i/item/9789289058506.
Honeine JL, Schieppati M, Gagey O, Do MC. The functional role of the triceps surae muscle during human locomotion. PLoS One. 2013;8(1):e52943.
Hulzinga F, Seuthe J, D’Cruz N, Ginis P, Nieuwboer A, Schlenstedt C. Split-Belt Treadmill Training to Improve Gait Adaptation in Parkinson’s Disease. Mov Disord. 2023 Jan;38(1):92-103.
Inacio M, Esser P, Weedon BD, Joshi S, Meaney A, Delextrat A, Springett D, Kemp S, Ward T, Izadi H, Johansen-Berg H, Dawes H. Learning a novel rhythmic stepping task in children with probable developmental coordination disorder. Clin Biomech (Bristol, Avon). 2023 Feb 3;102:105904.
Ivanenko Y, Shapkova EY, Petrova DA, Kleeva DF, Lebedev MA. Exoskeleton gait training with spinal cord neuromodulation. Front Hum Neurosci. 2023 May 11;17:1194702. doi: 10.3389/fnhum.2023.1194702.
Jin Y, Lee Y, Park S, Lee S, Lim C. Effects of Curved-Path Gait Training on Gait Ability in Middle-Aged Patients with Stroke: Protocol for a Randomized Controlled Trial. Healthcare 2023, 11, 1777.
Kasmi S, Zouhal H, Hammami R, Clark CCT, Hackney AC, Hammami A, Chtara M, Chortane SG, Salah FZB, Granacher U, Ounis OB. The Effects of Eccentric and Plyometric Training Programs and Their Combination on Stability and the Functional Performance in the Post-ACL-Surgical Rehabilitation Period of Elite Female Athletes. Front Physiol. 2021 Jul 2;12:688385.
Kariyawasam DS, D’Silva AM, Sampaio H, Briggs N, Herbert K, Wiley V, Farrar MA. Newborn screening for spinal muscular atrophy in Australia: a non-randomised cohort study. Lancet Child Adolesc Health. 2023 Jan 17:S2352-4642(22)00342-X.
Khobkhun, F., Santiago, P.R.P., Tahara, A.K. et al. An investigation of the contribution of different turn speeds during standing turns in individuals with and without Parkinson’s disease. Sci Rep 12, 22566 (2022).
Kuster MS. Exercise recommendations after total joint replacement. Sports Med. 2002;32:433–45.
Leach JM, Mellone S, Palumbo P, Bandinelli S, Chiari L. Natural turn measures predict recurrent falls in community-dwelling older adults: a longitudinal cohort study. Sci Rep. 2018 Mar 12;8(1):4316.
Lewis LK, Henwood T, Boylan J, Hunter S, Lange B, Lawless M, Milte R, Petersen J. Re-thinking reablement strategies for older adults in residential aged care: a scoping review. BMC Geriatr. 2021 Nov 30;21(1):667.
Lin TJ. Editorial Commentary: There Is No Standard for or Standardization of Postoperative Rehabilitation Protocols After Anterior Cruciate Ligament Reconstruction. Arthroscopy. 2023 Mar;39(3):590-591.
Lord SR, Close JCT. New horizons in falls prevention. Age Ageing. 2018 Jul 1;47(4):492-498.
Lowry K, Woods T, Malone A, Krajek A, Smiley A, Van Swearingen J. The Figure-of-8 Walk Test used to detect the loss of motor skill in walking among persons with Parkinson’s disease. Physiother Theory Pract. 2022 Apr;38(4):552-560.
Mancini M, El-Gohary M, Pearson S, McNames J, Schlueter H, Nutt JG, King LA, Horak FB. Continuous monitoring of turning in Parkinson’s disease: Rehabilitation potential. NeuroRehabilitation. 2015;37(1):3-10.
Mani H, Miyagishima S, Kozuka N, Inoue T, Hasegawa N, Asaka T. Development of the Relationships Among Dynamic Balance Control, Inter-limb Coordination, and Torso Coordination During Gait in Children Aged 3-10 Years. Front Hum Neurosci. 2021 Oct 28;15:740509.
Massardi, S., Pinto-Fernandez, D., Babič, J. et al. Relevance of hazards in exoskeleton applications: a survey-based enquiry. J NeuroEngineering Rehabil 20, 68 (2023).
Matsuda F, Mukaino M, Ohtsuka K, Tanikawa H, Tsuchiyama K, Teranishi T, Kanada Y, Kagaya H, Saitoh E. Biomechanical factors behind toe clearance during the swing phase in hemiparetic patients. Top Stroke Rehabil. 2017;24:177-182.
Mellone, S., Mancini, M., King, L.A. et al. The quality of turning in Parkinson’s disease: a compensatory strategy to prevent postural instability? J NeuroEngineering Rehabil 2016 13, 39.
Menz HB, Lord SR, Fitzpatrick RC. Acceleration patterns of the head and pelvis when walking on level and irregular surfaces. Gait Posture. 2003 Aug;18(1):35-46. doi: 10.1016/s0966-6362(02)00159-5. PMID: 12855299.
Morris L, Diteesawat RS, Rahman N, Turton A, Cramp M, Rossiter J. The-state-of-the-art of soft robotics to assist mobility: a review of physiotherapist and patient identified limitations of current lower-limb exoskeletons and the potential soft-robotic solutions. J Neuroeng Rehabil. 2023 Jan 30;20(1):18.
Novacheck TF, Gage JR. Orthopedic management of spasticity in cerebral palsy. Childs Nerv Syst 2007;23:1015-1031.
Odonkor CA, Thomas JC, Holt N, Latham N, Vanswearingen J, Brach JS, Leveille SG, Jette A, Bean J. A comparison of straight- and curved-path walking tests among mobility-limited older adults. J Gerontol A Biol Sci Med Sci. 2013 Dec;68(12):1532-9.
Palmowski, Y., Popovic, S., Schuster, S.G. et al. In vivo analysis of hip joint loading on Nordic walking novices. J Orthop Surg Res 2021 16, 596.
Patanè F, Rossi S, Del Sette F, Taborri J, Cappa P. WAKE-Up Exoskeleton to Assist Children With Cerebral Palsy: Design and Preliminary Evaluation in Level Walking. IEEE Trans Neural Syst Rehabil Eng. 2017 Jul;25(7):906-916.
Peterka RJ, Gruber-Fox A, Heeke PK. Asymmetry measures for quantification of mechanisms contributing to dynamic stability during stepping-in-place gait. Front Neurol. 2023 Apr 20;14:1145283.
Petrini M. (2023). The Effect of Treadmill Training Vs. Standard Physical Therapy on Gait in Individuals with Mild-Moderate Cerebral Palsy: A Meta-Analysis (Doctoral dissertation, California State University, Fresno).
Pierret J, Beyaert C, Vasa R, Rumilly E, Paysant J, Caudron S. Rehabilitation of Postural Control and Gait in Children with Cerebral Palsy: the Beneficial Effects of Trunk-Focused Postural Activities. Dev Neurorehabil. 2023 Mar 23:1-13.
Ribeiro de Souza C, Ávila de Oliveira J, Takazono PS, da Silva Rezende L, Silva-Batista C, Coelho DB, Teixeira LA. Perturbation-based balance training leads to improved reactive postural responses in individuals with Parkinson’s disease and freezing of gait. Eur J Neurosci. 2023 May 9.
Robinovitch SN, Feldman F, Yang Y, Schonnop R, Leung PM, Sarraf T, Sims-Gould J, Loughin M. Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. Lancet. 2013 Jan 5;381(9860):47-54.
Rodriguez K, Garcia SA, Spino C, Lepley LK, Pang Y, Wojtys E, Bedi A, Angelini M, Ruffino B, Bolley T, Block C, Kellum J, Swartout A, Palmieri-Smith RM. Michigan Initiative for Anterior Cruciate Ligament Rehabilitation (MiACLR): A Protocol for a Randomized Clinical Trial. Phys Ther. 2020 Dec 7;100(12):2154-2164.
Rosenkranz K, Rothwell JC. Modulation of proprioceptive integration in the motor cortex shapes human motor learning. J Neurosci. 2012 Jun 27;32(26):9000-6.
Rutz DG, Benninger DH. Physical Therapy for Freezing of Gait and Gait Impairments in Parkinson Disease: A Systematic Review. PM R. 2020 Nov;12(11):1140-1156.
Saito H, Sato M, Kobayashi M, Saito T, Shimura T, Yotsumoto K, Hanai Y, Tanizaki Y, Usuda S. Predictors of life-space mobility in patients with fracture 3 months after discharge from convalescent rehabilitation ward: a prospective longitudinal study. J Phys Ther Sci. 2023 Mar;35(3):223-229.
Shah VV, Jagodinsky A, McNames J, Carlson-Kuhta P, Nutt JG, El-Gohary M, Sowalsky K, Harker G, Mancini M, Horak FB. Gait and turning characteristics from daily life increase ability to predict future falls in people with Parkinson’s disease. Front Neurol. 2023 Feb 28;14:1096401.
Schalow G, Jaigma P. Cerebral palsy improvement achieved by coordination dynamics therapy. Electromyogr Clin Neurophysiol. 2005 Dec;45(7-8):433-45.
Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, Clemson L, Hopewell S, Lamb SE. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019 Jan 31;1(1):CD012424.
Sibley KM, Thomas SM, Veroniki AA, Rodrigues M, Hamid JS, Lachance CC, Cogo E, Khan PA, Riva JJ, Thavorn K, MacDonald H, Holroyd-Leduc J, Feldman F, Kerr GD, Jaglal SB, Straus SE, Tricco AC. Comparative effectiveness of exercise interventions for preventing falls in older adults: A secondary analysis of a systematic review with network meta-analysis. Exp Gerontol. 2021 Jan;143:111151.
Singer, J. C., Mansfield, A., Danells, C. J., McIlroy, W. E., & Mochizuki, G. (2013). The effect of post-stroke lower-limb spasticity on the control of standing balance: Inter-limb spatial and temporal synchronisation of centres of pressure. Clinical biomechanics, 28(8), 921–926.
Sozzi S, Schieppati M. Stepping in Place While Voluntarily Turning Around Produces a Long-Lasting Posteffect Consisting in Inadvertent Turning While Stepping Eyes Closed. Neural Plast. 2016;2016:7123609.
Sozzi S, Nardone A, Crisafulli O, Schieppati M. Podokinetic After-Rotation Is Transiently Enhanced or Reversed by Unilateral Axial Muscle Proprioceptive Stimulation. Neural Plast. 2019 Mar 11;2019:7129279.
Spildooren J, Vercruysse S, Desloovere K, Vandenberghe W, Kerckhofs E, Nieuwboer A. Freezing of gait in Parkinson’s disease: the impact of dual-tasking and turning. Mov Disord. 2010 Nov 15;25(15):2563-70.
Szopa, A.; Domagalska- Szopa, M. Postural Stability in Children with Cerebral Palsy. J. Clin. Med.2024,13,5263.
Thigpen MT, Light KE, Creel GL, Flynn SM. Turning difficulty characteristics of adults aged 65 years or older. Phys Ther. 2000 Dec;80(12):1174-87.
Turcato AM, Godi M, Giordano A, Schieppati M, Nardone A. The generation of centripetal force when walking in a circle: insight from the distribution of ground reaction forces recorded by plantar insoles. J Neuroeng Rehabil. 2015 Jan 9;12(1):4.
Turcato AM, Godi M, Giardini M, Arcolin I, Nardone A, Giordano A, Schieppati M. Abnormal gait pattern emerges during curved trajectories in high-functioning Parkinsonian patients walking in line at normal speed. PLoS One. 2018 May 11;13(5):e0197264.
van Dellen, F., Aurich-Schuler, T., Hesse, N. et al. Clustering trunk movements of children and adolescents with neurological gait disorders undergoing robot-assisted gait therapy: the functional ability determines if actuated pelvis movements are clinically useful. J NeuroEngineering Rehabil 2023 20, 71.
Ventura JD, Klute GK, Neptune RR. Individual muscle contributions to circular turning mechanics. J Biomech. 2015 Apr 13;48(6):1067-74.
Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018 Aug;49(8):1458-1460.
Vetrano D. La mappa della fragilità in Italia. Gradiente geografico e determinanti sociodemografici. (https://www.italialongeva.it/wp-content/uploads/2022/04/indagine-2022_italialongeva.pdf).
Wang ZH, Pan RC, Huang MR, Wang D. Effects of Integrative Neuromuscular Training Combined With Regular Tennis Training Program on Sprint and Change of Direction of Children. Front Physiol. 2022 Feb 10;13:831248.
Wright, M.A., Herzog, F., Mas-Vinyals, A. et al. Multicentric investigation on the safety, feasibility and usability of the ABLE lower-limb robotic exoskeleton for individuals with spinal cord injury: a framework towards the standardisation of clinical evaluations. J NeuroEngineering Rehabil 20, 45 (2023).
Zancan A, Beretta MV, Schmid M, Schieppati M. A new hip-knee-ankle-foot sling: kinematic comparison with a traditional ankle-foot orthosis. J Rehabil Res Dev. 2004;41:707-12.
Zancan A, Sozzi S, Schieppati M. Basic Spatio-temporal Gait Variables of Young and Older Healthy Volunteers Walking Along a Novel Figure-of-8 Path. Front Neurol. 2021 Jun 8;12:698160.
Zanotto T, Galperin I, Kumar DP, Mirelman A, Yehezkyahu S, Regev K, Karni A, Schmitz-Hübsch T, Paul F, Lynch SG, Akinwuntan AE, He J, Troen BR, Devos H, Hausdorff JM, Sosnoff JJ. Effects of a 6-week treadmill training with and without virtual reality on frailty in people with multiple sclerosis: Frailty rehabilitation in multiple sclerosis. Arch Phys Med Rehabil. 2024 Sep 26:S0003-9993(24)01262-0.
Ziemann U, Muellbacher W, Hallett M, Cohen LG (2001) Modulation of practice-dependent plasticity in human motor cortex. Brain 124:1171–1181.
Zoetewei D, Ginis P, Goris M, Gilat M, Herman T, Brozgol M, Thumm PC, Hausdorff JM, Nieuwboer A, D’Cruz N. (2024) Which Gait Tasks Produce Reliable Outcome Measures of Freezing of Gait in Parkinson’s Disease? J Parkinsons Dis. 14:1163-1174.
Figure 4. Animation of the device showing the dragging of the feet during the support phase and their realignment in space during the lifting phase
Here, the Google Scholar and ORCID page of the Founder of Prevent srl.
Back to contents index ☝
Back to the web site ☝